Frequently Asked Questions for Patients & Family
Everything You Need to Know About CardioClin™ and Coronary Artery Disease
We know heart health can feel overwhelming, especially when terms like “CAD” or “electro-mechanical risk” are new to you. This page offers clear answers to the most common questions from patients and families. Whether you want to know more about coronary artery disease or you’re wondering how the test works, what your results mean, or if it’s safe, you’ll find the information here.


What is CAD?
Coronary artery disease, also known as coronary heart disease (CHD) or ischemic heart disease (IHD), happens when the arteries supplying blood to your heart become narrowed due to plaque buildup. This restricts oxygen delivery to the heart and raises the risk of chest pain, heart attack, and sudden cardiac death¹.
Can coronary artery disease be reversed or cured?
CAD isn’t curable, but it is manageable. With the right mix of lifestyle changes, medications, and preventive care, people can slow the disease down and cut their risk of serious events like heart attacks².
Is CAD genetic?
Yes, if your parents had early-onset CAD, your own risk can be two to three times higher, making family history a risk factor³.
How is CAD diagnosed?
After you have been screened positive for coronary artery disease, doctors use several tools to diagnose coronary artery disease, depending on the situation:
- Physical stress tests
- Coronary artery calcium scoring (CACS)
- CT angiography (CCTA)
- Invasive coronary angiography (ICA)
- Electrocardiogram (ECG)
- Echocardiogram (Echo)
- Nuclear imaging such as SPECT and PET
These help assess how well blood is flowing and how blocked your arteries might be.
What is CAD also known as?
Coronary artery disease (CAD) is often referred to as coronary heart disease (CHD) or ischemic heart disease (IHD). These terms are frequently used interchangeably to describe conditions resulting from reduced blood flow to the heart due to plaque buildup in the coronary arteries¹˒². However, strictly speaking, CAD is a specific form of CHD/IHD, as it refers to atherosclerotic narrowing of the coronary arteries, whereas CHD and IHD may encompass a broader spectrum of ischemic cardiac conditions.
When is CAD typically diagnosed?
CAD is most often diagnosed in adulthood, typically in middle age or later, either when symptoms like chest pain occur or during routine health checks that reveal underlying risk factors⁶.
When does CAD begin?
The root cause of coronary artery disease, called atherosclerosis, can begin silently in childhood or adolescence. This plaque buildup progresses slowly over time, often without symptoms until later in life⁶.
Where does CAD occur?
CAD affects the coronary arteries, which are the blood vessels that wrap around the heart and deliver oxygen-rich blood to the heart muscle. When these arteries narrow, heart function can be compromised⁶.
Who gets CAD?
Anyone can develop CAD, but certain risk factors raise the likelihood. These include:
- age (especially over 40)
- high blood pressure
- smoking
- diabetes
- being overweight
- family history of heart disease⁶
Who treats CAD?
Coronary artery disease management often begins with your general practitioner (GP) or family doctor, but may involve heart specialists such as cardiologists. Diagnostic clinics and specialized heart centers may also help guide treatment depending on the condition’s severity.
Why does CAD occur?
CAD develops due to a combination of factors that damage artery walls, including high cholesterol, high blood pressure, smoking, diabetes, and unhealthy lifestyle habits¹. This leads to inflammation and plaque buildup, which narrows the arteries over time.
What’s the difference between CAD and atherosclerosis?
Atherosclerosis is the process where plaque builds up inside arteries throughout the body. Coronary artery disease is a specific type of atherosclerosis that affects the coronary arteries¹˒⁶, those that supply blood to the heart. In short, CAD is the result of atherosclerosis targeting the heart.
How does menopause affect a woman’s risk of coronary artery disease?
Menopause, particularly early menopause before age 45, can significantly increase a woman’s risk of developing CAD. Estrogen helps protect the heart by supporting healthy blood vessels and cholesterol levels. When estrogen levels decline during menopause, this protective effect is lost, which may accelerate atherosclerosis (plaque buildup in the arteries).
Women may also present with atypical or non-specific coronary artery disease symptoms, such as fatigue, shortness of breath, or nausea, rather than classic chest pain. Because these symptoms are often overlooked or misattributed to other causes, diagnosis may be delayed, highlighting the importance of early screening and open discussion of heart health during and after menopause.
What heart diseases can CardioClin™ help detect?
Coronary Artery Disease
How reliable is the CardioClin™ screening test compared to traditional CAD diagnostic tools like stress tests or Coronary Artery Calcium Scoring (CACS)?
The CardioClin™ test, powered by the EMCR Score™, has been validated in over 2,000 patients. At a 15% risk threshold, it demonstrated ~90% sensitivity, ~66% specificity, and a high negative predictive value (NPV ~95%), meaning it safely rules out obstructive CAD in most patients.
Compared with traditional screening tools:
- Stress tests: the EMCR Score™ delivers higher sensitivity and stronger NPV, reducing the risk of missed disease and unnecessary downstream testing.
- CACS: the EMCR™ Score shows comparable accuracy in ruling out CAD but adds important advantages: no radiation, portability, faster results (60 seconds), and use in both symptomatic and high risk patients with multiple CAD-associated risk factors.
- PTP/RF-CL: Unlike these population-based probability models, the EMCR Score™ integrates real patient-specific heart signals (SCG) with clinical factors, offering a more individualized risk assessment.
This combination makes CardioClin™ a versatile, non-invasive, and scalable option for earlier CAD detection.
Is the CardioClin™ screening device non-invasive?
Yes, 100% non-invasive and risk-free. Our screening test is designed with your comfort and safety in mind. It’s effective, and suitable for everyone, including those with medical implants like pacemakers.
No discomfort. No radiation.
There are no side effects and no known reasons why the test shouldn’t be used. Whether you’re prioritizing preventive care or managing heart health, our technology makes screening seamless and stress-free.
How does the CardioClin™ test work? What will I experience during it?
CardioClin™ is a smart, non-invasive tool designed to help healthcare professionals assess your risk for coronary artery disease (CAD), quickly, comfortably, and without any disruption to your care.
How It Works (in a nutshell)
Your doctor or nurse will guide you through a short and simple process. You’ll lie down on a medical bed and relax while a small sensor is gently placed on your chest. In about a minute, the system collects important data about your heart’s function and combines it with key health information to generate a personalized Electro-mechanical CAD Risk Score (EMCR Score™).
- Here’s What You’ll Do:
– Answer a few questions about your symptoms and health history
– Relax while the device gathers information: no pain, no radiation, no needles
- What Your Healthcare Provider Does:
– Reviews your symptoms and overall health
– Positions the CardioClin™ sensor on the center of your chest and starts the test
– Interprets your EMCR Score™ to determine next steps
- What You Get:
– A clear, evidence-based understanding of your current risk level for CAD: low, medium, or high
– Support for timely decisions and possible follow-up care, in case of a medium or high risk level, provided by your healthcare provider
CardioClin™ is especially helpful in everyday clinics, helping catch heart risk early without imaging or specialized equipment. It’s fast, safe, and designed to support better outcomes.
Risk Stratification Accuracy: The EMCR Score™ successfully stratified patients into five clinically actionable groups:
- Very Low Risk: CAD prevalence <5%;
- Low Risk: CAD prevalence 5 – >15%;
- Moderate Risk: CAD prevalence 15 – < 50%;
- High Risk: CAD prevalence – < 85%;
- Very High Risk: CAD prevalence > 85%
High-Risk Screening: EMCR Score™ could detect CAD risk in high risk patients with multiple CAD-associated risk factors, a major limitation of current screening tools.
How long does the CardioClin™ test take?
The CardioClin™ heart screening test is fast and comfortable. The full process, from getting set up to receiving your results, takes just 5 to 10 minutes. And the actual test only requires 60 seconds of heart data, making it quick, gentle, and completely non-invasive. That means no stress, no waiting, and no recovery time, just a smooth experience for you and an efficient screening tool for your healthcare provider.
Do I need to prepare for the CardioClin™ test?
No extensive preparation is required. Just make sure the sensor can make direct contact with clean skin, avoiding thick body hair or clothing in the test area helps ensure the most accurate results.
Will I need more than one CardioClin™ test?
You might not need frequent check-ups, but heart health is an ongoing journey. Coronary artery disease (CAD) risk can grow over time, especially if you have risk factors like diabetes, high blood pressure, or high cholesterol, or if you’ve smoked in the past. That’s why we recommend screening every 2–3 years, particularly if you have known risk factors. Early detection makes a big difference, and CardioClin™ helps make that easy.
How fast do I get my CardioClin™ results?
Once your test data is collected, the CardioClin™ cloud AI system analyzes it and delivers your results in just 60 seconds. That means you and your provider can discuss what’s next without delay.
What If my results show something unusual?
CardioClin™ is a risk screening tool, meaning it helps spot potential signs of coronary artery disease (CAD). If your results suggest elevated risk, your healthcare provider will guide you through the next steps, which may include additional diagnostic tests to get a clearer picture.
Is CardioClin™ a replacement for other CAD tests?
CardioClin™ is designed to complement existing risk assessment protocols. It helps providers quickly assess whether someone might be at risk for CAD and determine if further testing is needed.
Does the CardioClin™ device store or send my health data?
Yes, the system is fully GDPR and HIPAA-compliant, meaning it meets strict standards for keeping your medical data safe and protected.
Who can see my test results?
Only your healthcare provider, no one else. Your results stay private and are used strictly for your care
Is my data shared with others or used for research?
Your personal information is never shared with third parties. In some cases, anonymized data, with all identifying details removed, is used to improve the system’s ability to detect heart risks. This helps make CardioClin™ smarter for everyone, without compromising your privacy.
How does the CardioClin™ test compare to other heart screening tools?
When it comes to detecting coronary artery disease (CAD), most traditional screening tools lean heavily on symptom-based checklists or statistical models like Pre-Test Probability (PTP) and Risk Factor–Clinical Likelihood (RF-CL). These tools provide a statistical likelihood based on factors like age, gender, and known symptoms without using any specific clinical data like seismocardiogram data used by CardioClin. However, they can only be used if you already have symptoms, and even then, they often overestimate the risk.
Other diagnostic tests like stress ECGs or coronary artery calcium scoring (CACS) have a similar sensitivity as CardioClin™, but they are mostly used for individuals with CAD associated risk factors to rule out coronary artery disease instead of individuals without CAD symptoms.
That’s where the EMCR Score™ from our CardioClin(™) device changes the game:
- Works for both symptomatic, and high risk patients with multiple CAD-associated risk factors
- Helps doctors confirm or rule out CAD risk
- Is non-invasive, fast, and easy to use
By offering reliable insights early, even in patients who may otherwise be undiagnosed, CardioClin™ empowers smarter, more personalized heart care.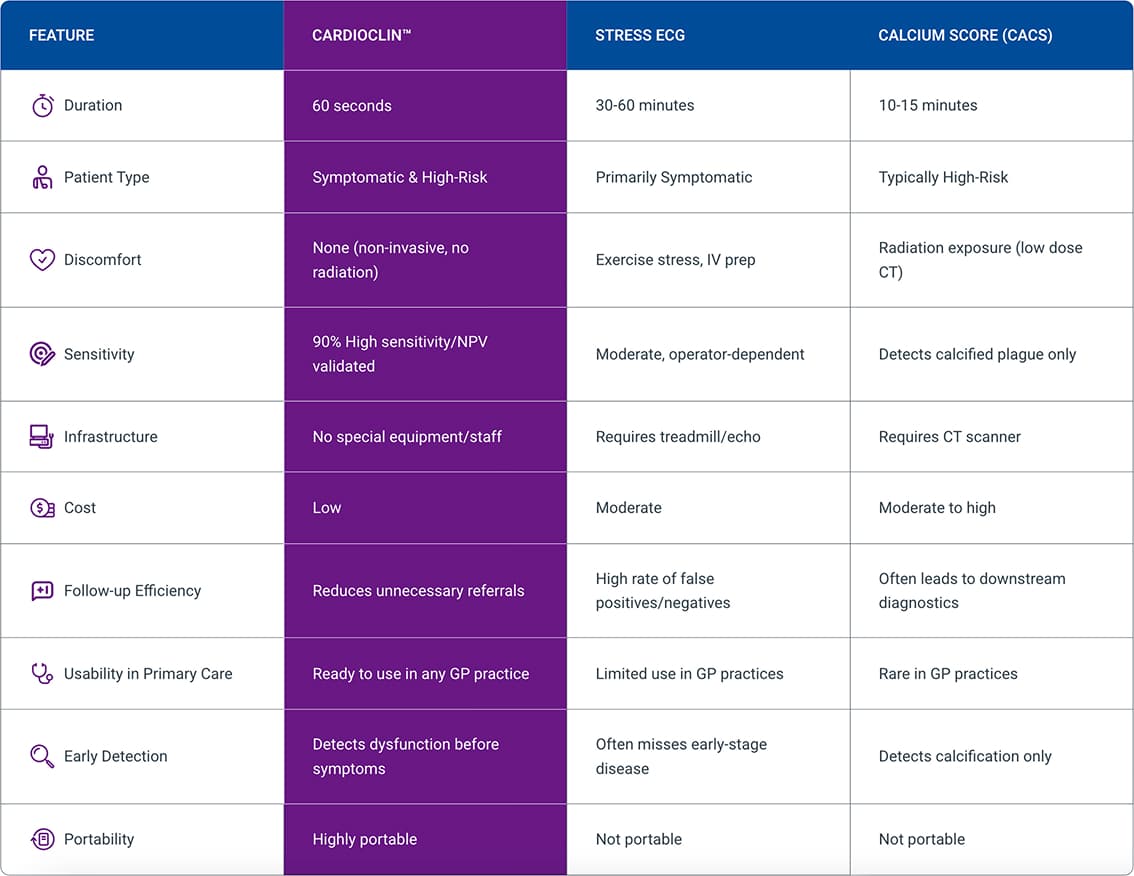
Who can see my test results?
Only your healthcare provider, no one else. Your results stay private and are used strictly for your care
Is my data shared with others or used for research?
Your personal information is never shared with third parties. In some cases, anonymized data, with all identifying details removed, is used to improve the system’s ability to detect heart risks. This helps make CardioClin™ smarter for everyone, without compromising your privacy.
References
- Institute of Medicine. 2010. Cardiovascular Disability: Updating the Social Security Listings. Washington, DC: The National Academies Press. https://doi.org/10.17226/12940
- Shahjehan RD, Sharma S, Bhutta BS. Coronary Artery Disease. [Updated 2024 Oct 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564304/
- Scheuner, M., Whitworth, W., McGruder, H. et al. Expanding the definition of a positive family history for early-onset coronary heart disease. Genet Med 8, 491–501 (2006). https://doi.org/10.1097/01.gim.0000232582.91028.03
- National Heart, Lung, and Blood Institute. Stroke: Causes [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; [cited 2025 Aug 6]. Available from: https://www.nhlbi.nih.gov/health/stroke/causes
- Mayo Clinic. Stroke: Symptoms and causes [Internet]. Rochester (MN): Mayo Foundation for Medical Education and Research; [cited 2025 Aug 6]. Available from: https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113
- Luca AC, David SG, David AG, Țarcă V, Pădureț IA, Mîndru DE, Roșu ST, Roșu EV, Adumitrăchioaiei H, Bernic J, Cojocaru E, Țarcă E. Atherosclerosis from Newborn to Adult-Epidemiology, Pathological Aspects, and Risk Factors. Life (Basel). 2023 Oct 14;13(10):2056. doi: 10.3390/life13102056. PMID: 37895437; PMCID: PMC10608492